Part 1 of 2
This May marks the 10th anniversary of the UW’s Coulter Translational Research Partnership in Biomedical Engineering, which has helped propel dozens of UW inventions from the lab toward clinical use. The UW was one of the first 10 universities to pioneer the program, which funds projects that address unmet clinical needs in patient care.
The Coulter program awards one-year, $100,000 grants to teams led by a UW faculty member and a clinician, and whose focus is on transferring their research into practice.
“We fund projects with a high likelihood of commercial success,” says Kathie Jordan, director of UW’s Coulter program. “Often they are in the early stage proof-of-concept category, and they are ready to move to next level.”
To date, the UW Coulter program has given $6.6 million in awards, which has resulted in some $780 million in follow-on funding from other sources, such as venture capitalists and research foundations, Jordan says.
To further support the success of the program awardees, Coulter partners with UW’s CoMotion (formerly the UW Center for Commercialization or C4C), Institute of Translational Health Sciences and the Washington Research Foundation.
Two of Coulter’s most recent successes come from the Department of Bioengineering, with technologies that have spun out into Nexgenia and another new company.
In this issue, BioE enews takes a look at the core technology that transferred to Nexgenia.
Nexgenia builds on BioE’s smart polymers and cell separation technology
UW bioengineers James Lai and Patrick Stayton, co-founders of Nexgenia, and their collaborators invented polymer-based nanotechnology to make clinical tests that are more sensitive, work faster and have better cell separation, with the goal of allowing earlier detection of cancer, infectious disease and other illness.
“For research that can potentially address unmet clinical need, the Coulter program actually accelerates the process amazingly,” says Dr. Lai, research assistant professor in bioengineering. Dr. Lai says he and his co-inventors had been trying to promote the technology that spun out into Nexgenia for at least a few years. “It never got realized until 2010, when we received funding through the Coulter program,” Dr. Lai says. “The key piece is the program, which is not only the funding, but also the services and expert resources they provide, which helped us look at whether the idea was feasible or not.”
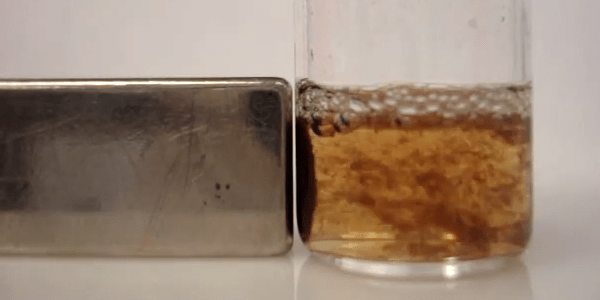
The core of Nexgenia’s technology is the use of smart polymers combining antibodies and magnetic nanoparticles. Very small magnetic nanoparticles bind to biomarkers dramatically better than current microbeads, but their size makes them too small to be attracted by a magnet. Nexgenia’s smart magnetic nanoparticles can switch between being individual particles that are good at recognizing targeted molecules and forming large particulate aggregates with dimensions big enough to be rapidly pulled over to a magnet and separated from the rest of the sample.
Fast and easy separation is a key advantage enabled by the polymer they developed. The smart particles can be small and mix with specimen solution to find target biomarkers at room temperature, but making a small, simple change in conditions, such as altering temperature, pH or salt level, causes the particles to immediately form large aggregates that can be pulled to a magnet, key biomarkers in tow.
In October 2014, Nexgenia, which uses lab space in the New Ventures Facility on the UW campus, announced that it would focus its efforts on the cell separation technology for use in personalized immunotherapy. Immunotherapy uses the body’s own immune system to help fight cancer and other diseases.
Nexgenia plans to use the polymer technology to quickly and accurately sort out the key immune cells from a patient’s blood that can be re-engineered, and returned to the patient’s body for treatment.
“It’s truly exciting for me personally, knowing that there’s a potential that my work can make an impact clinically,” Dr. Lai says. “The work that we spun out to Nexgenia is a technology that can potentially make the clinical diagnostic more sensitive. It can basically identify more patients who need help. This is not a trivial thing.”
Nexgenia continues to receive pilot funding, including a $1.2 million Small Business Innovation Research grant in 2013 and grants from UW’s CoMotion, the Life Sciences Discovery Fund and the Washington Research Foundation in fall 2014.
Read Part 2 to learn about a new drug screening platform designed to test for cardiac toxicity and ensure safer drugs get to market.
Article by Lia Unrau