Reprinted here. Original story
One researcher combats cancer with the help of UW doctors and tools developed by his colleagues.
By: Chelsea Yates
Photos: Dennis Wise / University of Washington
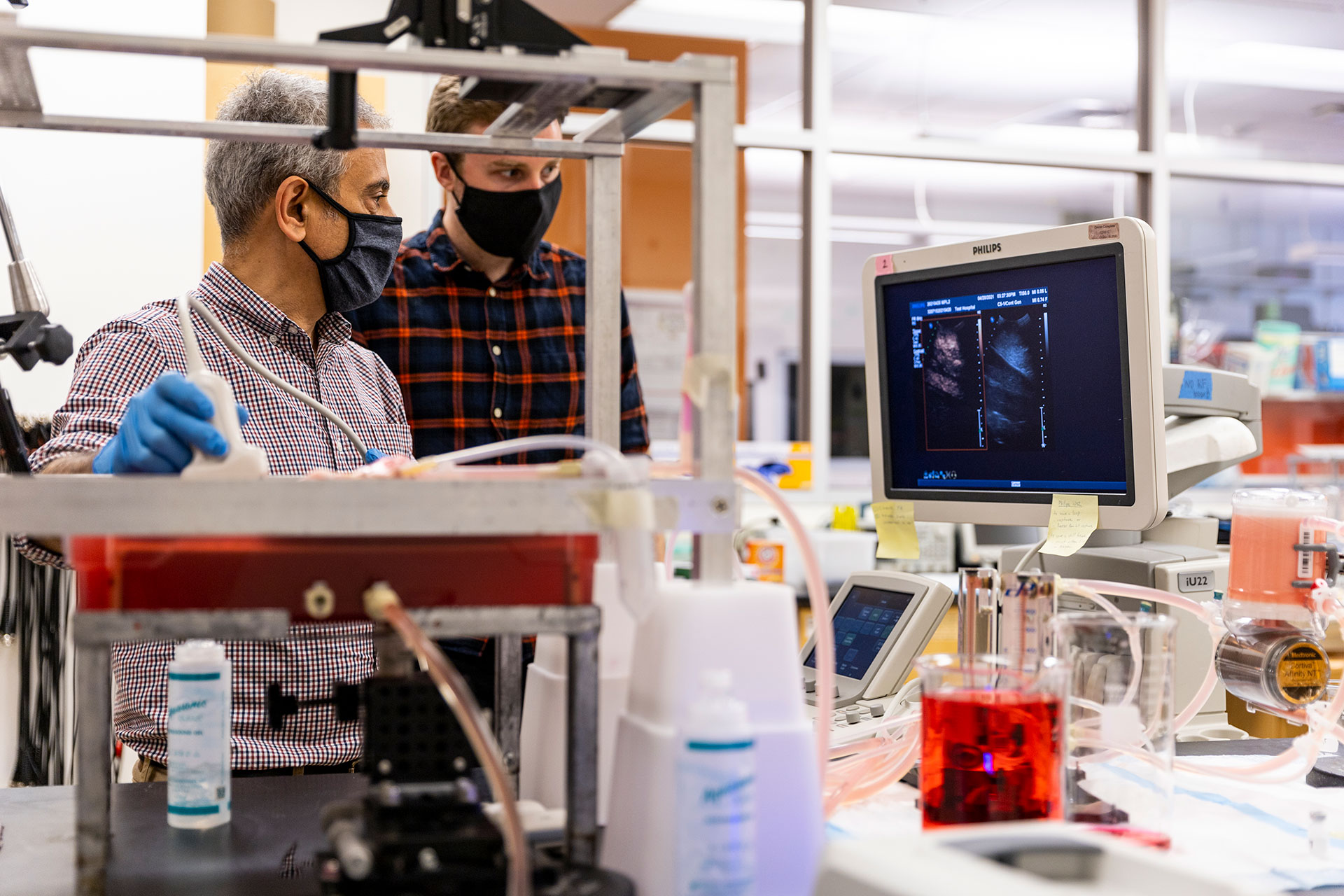
Top image: Mike Averkiou, left, Barry Lutz, center, and Manjiri Dighe, right, during a recent contrast-enhanced ultrasound of Lutz’s liver. The image on the left side of the screen depicts microbubble contrast agents in the blood flow of Lutz’s liver, confirming the absence of metastatic lesions. The image on the right is a normal ultrasound image showing liver tissue.
On June 26, 2019, Barry Lutz received news no one wants to get: he had late stage colon cancer.
“It was a complete surprise,” the associate professor of bioengineering says. The median age for colon cancer diagnosis in men is 68; Lutz was 44. Neither he nor anyone in his family had a history of colon cancer.
Lutz’s care team, led by oncologist Eddie Marzbani at UW Medical Center – Northwest, set to work. Lutz had surgery to remove the cancer and spent the next three months in treatment.
Lutz finished chemotherapy and on December 22, he had a CT scan to serve as a clean baseline for future monitoring. The next day, he moved with his family to Texas to be near relatives and to resume a sabbatical, which had been interrupted by his cancer diagnosis. Things were looking up.
But a few days later, Dr. Marzbani called with bad news. Instead of clearing him, the CT scan showed a mass in his liver.
Though the scan could detect the mass, it couldn’t determine if the mass was malignant. So Lutz and his medical team were looking at a second surgery — in the liver this time. But it was risky. The mass appeared too big to remove completely and, if it was cancerous, the likelihood that cancer would spread was high. Plus, surgery could undermine Lutz’s already weakened immune system.
At this point, Lutz says, everything seemed “pretty dark.”


Your Content Goes Here

Dighe, left, prepares the microbubble contrast agent while Averkiou attaches an articulated arm to the bed to keep the ultrasound probe stationary during the scan. Lutz, center, photographs the process.

“I have a lot to be thankful for at UW Medicine — from oncology to surgery and two great UW technologies. They all came together to give me a real gift.”