Need for treatments drives new technologies to grow human organs from scratch
As internal organs go, the human liver has a rare superpower – the ability to regenerate itself. But it’s not invincible. A liver transplant remains the only treatment for people with diseased or damaged livers that are beyond self-repair. In 2021, over 9,000 Americans received liver transplants, but without enough donor supply, many were left on the waitlist.
To meet this clinical need, UW researchers are working to reveal in detail how human livers form, with the ultimate goal of growing new organs in the lab.

Kelly Stevens
University of Washington bioengineer Kelly Stevens, whose research focuses on mapping human organs and engineering artificial human tissues, has been named an Allen Distinguished Investigator by The Paul G. Allen Frontiers Group, a division of the Allen Institute. The award will support her work to map and understand how human livers develop.
The $1.3 million, three-year grant will allow the Stevens lab to explore the complex set of factors involved in liver formation. The project will build on the Stevens lab’s expertise in building organoids (3D clusters of organ tissue), synthetic biology and 3D bioprinting.
“This will allow us to take major steps towards the dream of building human organs for use as ‘replacement parts’ for our bodies,” said Stevens, an assistant professor in the UW departments of bioengineering and of laboratory medicine & pathology. She is also a faculty member at UW Medicine’s Institute for Stem Cell & Regenerative Medicine.
“Our ultimate goal is to both “read” how human livers grow in our bodies, and then “write” – or build – livers in a dish that can be used for human therapy.” – Kelly Stevens
Much about how the liver forms and its ability to self-heal remains a mystery. Researchers have learned that as the liver grows, a well-orchestrated process creates distinct areas within the structure. Each location has its own type of environment tailored to carry out vital functions, such as producing human proteins, cleaning the blood or metabolizing fats and sugar.
Stevens and her team will investigate the complex network of factors that interact and give rise to the liver’s form and some of its 500 diverse functions. The project will explore the interplay of biochemical cues, genetics, mechanical forces, blood supply factors and cell environments to reveal their collective influence on how liver cells mature, organize into specific locations and take on essential tasks. Researchers have only recently started looking at the role of mechanical forces and blood supply in liver regeneration.
A library of plug-and-play environments
Stevens’ team will engineer synthetic technologies that can “rebuild” each of the biochemical, genetic, mechanical, and blood vessel aspects that are found in developing human livers in utero, in a dish. Using this library of plug-and-play environments, they will coax liver cells to communicate, multiply and organize into different cell types, to ultimately “grow” a mini human liver.
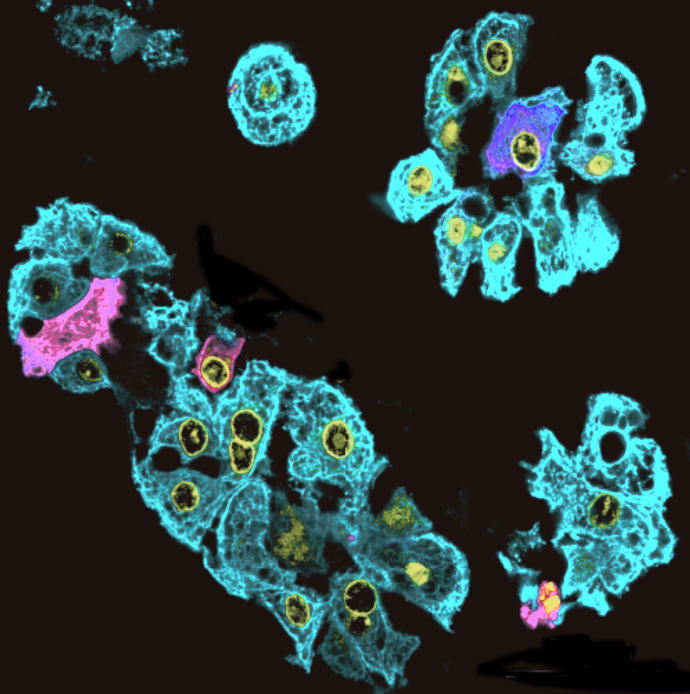
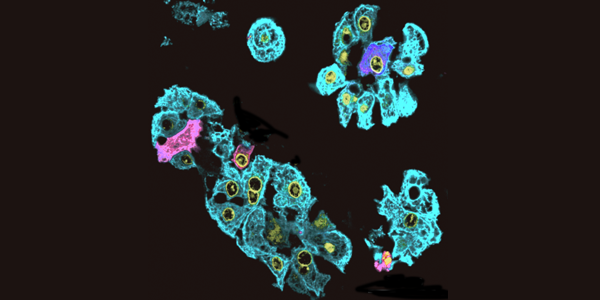
Liver cells image by Sarah Saxton
This work will build on previous advances from the Stevens lab. In 2019, Stevens and colleagues reported on 3D bioprinted tissues with entangled vascular networks for air and blood. In 2020, the Stevens lab and collaborators reported on their 3D printed fluid systems that supply penetrating heat in patterns that trigger gene expression in human livers. And in 2021, Stevens and colleagues reported on their sci-Space technology, a technique that tracks cell positions and gene expression over time in a developing embryo. In a current study, her lab is examining the fundamental role of mechanical forces in shaping or hindering the re-formation of livers.
For some aspects of this project, the Stevens lab will collaborate with Ludovic Vallier of the University of Cambridge, an expert in stem cells, liver organoids and genome editing, and Dr. Robert Schwartz of Weill Cornell Medicine, a clinician and expert in stem cell biology and tissue vascularization.
“Our ultimate goal is to both “read” how human livers grow in our bodies, and then “write” – or build – livers in a dish that can be used for human therapy,” Stevens said.
The researchers note that the technical innovations the team is creating for building liver will also be useful for generating other organs, such as heart, kidney, pancreas and brain.
A national leader in mentorship, community building and inclusivity
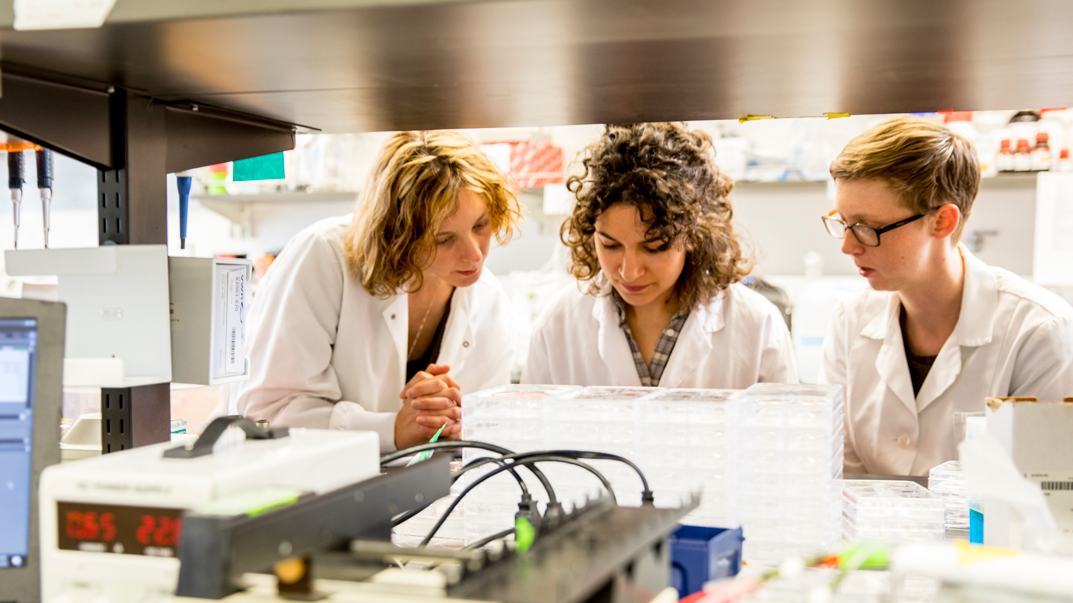
Kelly Stevens, left, in her South Lake Union lab with graduate student mentees Colleen O’Connor, center, and Eileen Brady, right.
Stevens is a national leader in mentorship, community building and inclusivity in science. In 2021, she was elected to co-lead the National Academies of Science, Engineering, and Medicine 2021-2023 New Voices Cohort, an initiative to bring diverse ideas about critical and emerging challenges to the work of the National Academies. She also co-founded and co-leads the nationwide biomedical engineering UNITE movement, which includes about 400 biomedical engineering faculty working to improve racial and ethnic diversity in higher education. In addition, Stevens co-leads the Genentech Research Awards Program, which grants research funding to underrepresented minority faculty in biomedical engineering. At UW, she is a champion of inclusivity within her own lab and through service on various committees, including UW BioE’s Justice, Equity, Diversity and Inclusion (JEDI) committee.
The Allen Distinguished Investigator Award supports researchers around the world whose work has the potential to accelerate scientific discoveries or launch entirely new avenues of exploration.
Article by Lia Unrau